I’m sure that most of you will have heard in the news over the last few weeks about Angelina Jolie undergoing a preventive double mastectomy because of her very high risk of developing breast cancer, having inherited a breast cancer gene from her mother.
I’m sure that most of you will have heard in the news over the last few weeks about Angelina Jolie undergoing a preventive double mastectomy because of her very high risk of developing breast cancer, having inherited a breast cancer gene from her mother.
One of Angelina Jolie’s aims when she went public with her story was to raise awareness about inherited breast cancers and to encourage women with a family history of breast or ovarian cancer to go to see their doctors to determine their own personal risk and to get help to make informed choices about how to manage this risk.
Her story has definitely raised public awareness – it’s got people talking and it’s got people asking questions – I’ve certainly been asked a few. I hope to be able to answer some of these questions here.
What are the breast cancer genes?
We know that some women carry a faulty gene that gives them a higher risk than normal of developing breast cancer.The genes BRCA1 (breast cancer gene 1) and BRCA2 (breast cancer gene 2) are the most common faulty genes but there are others. And it is possible to carry more than one faulty gene.
Just to explain, everyone carries the BRCA 1 and the BRCA 2 genes. They’re from a group of genes called ‘tumour suppressor genes’. These genes are there to help keep breast cells growing normally and to repair any damage to breast cells. It’s when the genes have mutations (or faults) in them that they don’t work properly and that the risk of developing breast cancer increases.
Just because you carry a faulty gene doesn’t mean that you’ll definitely develop breast cancer, but your risk is increased. And, the actual risk can be different for each woman. Angelina Jolie carries the BRCA 1 faulty gene and, on average, women who carry this faulty gene have a 65% risk of developing breast cancer. For Angelina Jolie, her doctors estimated that her risk of breast cancer was 87%. It’s a bit complicated but researchers think that other mutations (other faults) in pieces of genetic material, on top of the faulty breast cancer gene, can make the risk of breast cancer even higher in some women.
Some other important things to say are that if breast cancer does develop because of a faulty gene, then it tends to develop at a younger age. And, it’s also more likely to develop in both breasts rather than just one breast.
What’s the link with ovarian cancer?
Women who have a faulty BRCA 1 or BRCA 2 gene also have an increased risk of developing ovarian cancer. These genes are also involved in controlling the normal growth and repair of the cells in the ovaries – so again, if there is a mutation (a fault) in the gene, then this control can be lost. And, in the same women, the risk of colon, pancreatic, thyroid and melanoma skin cancer is also increased.
Men and the breast cancer genes
We know that men who carry the faulty BRCA 2 gene have an 80 times higher than average chance of developing breast cancer. This means that by the time they’re 80, the chance of them developing breast cancer is about 8%.Remember – breast cancer in men is less common than breast cancer in women.
If they carry the faulty BRCA 1 gene, then this actually increases the man’s risk of prostate cancer – they’re 7 times more likely to develop prostate cancer than men who don’t carry the faulty gene.
 Is breast cancer always due to faulty genes?
Is breast cancer always due to faulty genes?
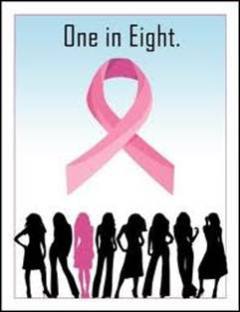
Breast cancer is one of the most common cancers in the world. A woman’s lifetime risk of developing breast cancer is around 1 in 8.
Most breast cancers are not due to genetics – they don’t develop because of the woman carrying faulty genes. Genetics are involved in only around 1 in 20 women with breast cancer.
Other risk factors for breast cancer include:
- Increasing age – most breast cancers occur in women over the age of 50. For every 10 years of increasing age, your risk of developing breast cancer roughly doubles.
- Being overweight – especially if you’ve already gone through the menopause.
- A lack of regular physical activity in your life.
- Regularly drinking alcohol over the recommended limits.
- Not having children, or having your first child when you’re over the age of 30.
- Taking hormones – it’s a bit complicated but your risk of breast cancer may be slightly increased if you take the combined oral contraceptive pill over the age of 35 (that’s the pill containing both oestrogen and progesterone). And there’s also a slightly increased risk of breast cancer if you take hormone replacement therapy. Combined HRT (HRT containing oestrogen and progesterone) carries a higher risk than oestrogen-only HRT. And the risk increases the longer you’ve been taking the HRT. When you haven’t taken HRT for five years, then your risk of breast cancer drops to that of a woman who has never taken HRT.
And I’m sure that there are other risk factors involved that we don’t yet know about – or that we may never know about.
If I carry a faulty breast cancer gene, what’s my risk of passing it on to my children?
If you remember, you inherit half your genes from your mother and half your genes from your father. So, if you carry a faulty breast cancer gene, there’s a 50:50 chance that you’ll pass it on to each child that you have. This means that if one of your family members has a faulty breast cancer gene, all of the family members will not necessarily have inherited it.
And, just to say, that both men and women can carry the faulty breast cancer gene and so can pass it on to their children.
I have someone in my family who has had breast cancer. How do I know if it was due to a faulty gene?
Breast cancer is common. So people will often have someone in their family who has been diagnosed with the disease. But, if there is a history of breast cancer in the family, it won’t usually be because of faulty breast cancer genes being passed on through the generations. Most of the time, the breast cancer in the family will have occurred by chance, perhaps under the influence of some other breast cancer risk factors that we’ve talked about.
The risk of breast cancer in your family having been caused by a faulty gene (being a true hereditary breast cancer) becomes greater if:
- You have blood relatives (mother, grandmothers, sisters, aunts) on either your mother’s side of the family or your father’s side of the family who developed breast cancer before the age of 50.
- There is a history of both breast and ovarian cancer in the family, particularly if these cancers occurred in one person.
- Any woman in your family has developed breast cancer in both breasts.
- A man in your family has had breast cancer.
- You are from a certain ethnic background – for example the Ashkenazi Jewish community.
- You have a number of relatives who have had breast cancer. The more relatives that are affected in your family, the greater the chance that faulty genes are involved.
The bottom line is, if you are worried that breast cancer may run in your family, go and talk to your doctor. Try to map out a family tree before you go and mark on it the relatives who have had breast cancer. Your doctor will be able to discuss your risk with you. They may refer you on to see a specialist for genetic counselling and assessment.
If a woman is found to carry a faulty breast cancer gene, what will happen?
Remember, it’s still not certain that you will develop breast cancer if you carry the faulty gene. You can look at other risk factors for breast cancer as well and try to minimise those – like the lifestyle risk factors that we talked about: try to maintain a healthy weight and eat a healthy diet, try to do plenty of physical activity, don’t drink too much alcohol and don’t smoke.
But also more frequent screening for breast cancer is usually advised – you can develop a screening plan with your doctor – we’re talking about breast examinations, mammograms and other scans like MRI scans starting at a much earlier age, and happening more regularly than would be usual for breast cancer screening.
Various hormonal therapies may also be considered and they may help to reduce the risk of developing certain breast cancers in some women who carry the faulty breast cancer gene.
And then, there is the option of ‘protective – or prophylactic – surgery’ like Angelina Jolie has had. Basically removing the healthy breasts and so removing the risk of cancer developing to a large extent. We know that prophylactic breast surgery (a bilateral mastectomy) can reduce a woman’s risk of developing breast cancer by about 97%. The surgery can’t remove every single cell of breast tissue so that’s why it’s not a 100% reduction in risk.
Surgery to remove the ovaries may also be discussed because of the risk of developing ovarian cancer. In Angelina Jolie’s case, she says that she started with the breast surgery because her risk of developing breast cancer was higher (87% compared to 50% for ovarian cancer) and also because the breast surgery is more complex.
Regardless of any family history of breast cancer, every woman should be ‘breast aware’
 As a woman, you know your body best and you are the person who is likely to notice any changes in your breasts that may indicate possible breast cancer. In particular, you need to look out for:
As a woman, you know your body best and you are the person who is likely to notice any changes in your breasts that may indicate possible breast cancer. In particular, you need to look out for:
- Changes in breast size or shape.
- Changes in the texture of the breast skin like puckering or dimpling of the skin.
- A nipple that becomes inverted (turns in on itself).
- A lump or thickening that you can feel in the breast.
- Redness or a rash on the skin of the breast or around the nipple.
- Discharge from one or both nipples.
- Constant pain in a breast or in one of your armpits.
- A swelling that develops in one of your armpits or around a collarbone.
If you notice any of these changes, then don’t wait, go and get it checked out by a doctor.
And also, if you are worried about your risk of breast cancer because there is a history in your family, again, go and talk to your doctor. In Switzerland, your gynaecologist is probably the best person to talk to. For those of you living in the Geneva region, your gynaecologist may refer you to the Breast Centre at the University Hospital where a mulidisciplinary team is available including genetic specialists as needed. To find out more information about this centre, click here.
The Swiss Cancer League also have also produced an information leaflet in English about breast cancer which has some useful contact details click here.
And there’s another leaflet in English including information about breast cancer screening in Switzerland click here
Let’s use Angelina Jolie’s story as it was intended – as an opportunity to stimulate conversation and raise awareness about breast cancer. Please feel free to pass this on to others who may be interested.
By Dr Michelle Wright